Healthy Montana Kids (HMK) and CHIP Dental Services Manual
Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
If you experience any difficulty opening a section or link from this page, please email the webmaster.
How to Search this manual:
This edition has three search options.
- Search the whole manual. Open the Complete Manual tab. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials)". The search box will show all locations where denials are discussed in the manual.
- Search by chapter. Open any chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials"). The search box will show where denials are discussed in just that chapter.
- Site search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs site specific search page.
Prior manuals may be located through the provider website archives.
Healthy Montana Kids (HMK) and CHIP Dental Services Manual
Updated 08/22/2025
Healthy Montana Kids (HMK) and Children's Health Insurance Program (CHIP) Manual
To print this manual, right click your mouse and choose "print". Printing the manual material found at this website for long-term use is not advisable. Department Policy material is updated periodically and it is the responsibility of the users to check and make sure that the policy they are researching or applying has the correct effective date for their circumstances.
Update Log
Publication History
This publication supersedes all previous Physician-Related Services handbooks. Published by the Montana Department of Public Health & Human Services, January 2005.
Updated January 2003, October 2015, December 2015, August 2017, and August 2025
CPT codes, descriptions and other data only are copyright 2014 American Medical Association (or such other date of publication of CPT). All Rights reserved. Applicable FARS/DFARS Apply.
Update Log
08/22/2025
Deleted bulleted text in HMK/CHIP Reimbursement - Dental Plan section in the Reimbursement, covered, and Non-Covered Services chapter.
- Pre-approved medically necessary dental and orthodontic services only related to craniofacial anomaly or cleft palate are covered under the child's medical portion of HML/CHIP. This is handled through Children's Special Health Services.
08/03/2017
Healthy Montana Kids (HMK) and Children's Health Insurance Program (CHIP) Dental Services Manual converted to an HTML format and adapted to 508 Accessibility Standards. Additionally, updates were made throughout the manual.
12/31/2015
HMK and CHIP Dental, January 2016, HELP Plan-Related Updates and Others
10/05/2015
HMK and CHIP Dental, September 2015: Entire Manual
01/14/2003
HMK and CHIP Dental
Beginning in 2013, the format of the manual was changed. The manual was updated in July.
End of Update Log Chapter
Table of Contents
Key Contacts and Websites
General Information
Enrollment Information
Getting Assistance
Adjustment Request Form and Dental Claims Forms
Department Responsibilities
Fiscal Agent Responsibilities
Verifying HMK/CHIP Eligibility
How to Verify Eligibility
Failure of Eligible HMK/CHIP Member to Notify Provider of HMK/CHIP Eligibility
HMK/CHIP Dental Benefit Plan
Reimbursement, Covered, Non-Covered Services
HMK/CHIP Reimbursement - Dental Plan
Determining HMK/CHIP Reimbursement
Billing the Member
Covered Services
Non-Covered Services
Usual and Customary Charges
No-Show Appointments
Medical Necessity
Billing Procedures
Important Billing Guidelines
Coding Requirements - Current Dental Terminology, Dental Procedure Codes
Paper Submission of Claims - ADA Claim Form
Provider Specialty Codes
Authorized Signatures
Where to Send Claims
Timely Filing
Follow-Up on Claim Resolution
How to Appeal Timely Filing Denials
Billing Tips to Avoid Timely Filing Denials
The Remittance Advice
How to Resubmit a Dental Claim
Adjustments
Provider Responsibilities
Provider Number
Changes in Provider Enrollment
Recertification
Provider Participation
Accepting HMK/CHIP Members and Provider-Member Relationship
Record Keeping, Retention, and Access
Appendix A: Forms
Definitions and Acronyms
Index
End of Table of Contents Chapter
Key Contacts and Websites
Hours for Key Contacts are 8 a.m. to 5 p.m. Monday through Friday (Mountain Time), unless otherwise stated. For additional contacts and websites, see the Contact Us link in the left menu on the Montana Healthcare Programs Provider Information website.
Adjustment Requests
The Adjustment Request form and a sample dental form are on the Forms page of the Provider Information website.
American Dental Association (ADA) dental claim forms and the Current Dental Terminology (CDT) procedure code manual are not supplied by Conduent or DPHHS.
To order from the ADA, call 1-800-947-4746 or order online.
Dental Claims
Send dental claims to:
Conduent Claims Processing
P.O. Box 8000
Helena, MT 59604
1 (406) 442-2819 Fax
Dental Accident-Related Claims
Dental services related to an accident need to be reported to the HMK/CHIP Dental program officer for pre-approval. Dental accidents are covered through the child’s HMK/CHIP medical insurance plan. Providers of these services should contact the HMK/CHIP program officer for additional information.
Dental Program Officer
HMK/CHIP
P.O. Box 202951
Helena, MT 59620-2951
1 (406) 444-7045 Phone
1 (406) 444-1861 Fax
American Dental Association (ADA)
http://www.ada.org/en/
Information Available: The leading source of oral health related information for dentists and their patients.
Healthy Montana Kids (HMK)
https://dphhs.mt.gov/HMK
Information Available: Information on HMK/CHIP including eligibility, family and provider resources, enrollment, covered services, approved providers, copayments, how to become a provider, how to get a provider manual, and frequently asked questions.
InsureKidsNow.Gov
http://insurekidsnow.gov
Information Available: All states’ CHIP coverage and Find a Dentist feature.
End of Key Contacts and Websites Chapter
General Information
Enrollment Information
For information about becoming a Healthy Montana Kids (HMK) provider, contact Provider Relations or the HMK/CHIP Dental Unit.
Provider Relations
P.O. Box 4936
Helena, MT 59604
1 (800) 624-3958 In/Out of state
1 (406) 442-1837 Helena
HMK/CHIP Dental Unit
1 (877) 543-7669, X7045
1 (406) 444-7045
Dental services related to a trauma need to be reported to the HMK/CHIP Dental program officer for pre-approval. Dental trauma may be covered through the child’s HMK/CHIP medical benefit. Providers of these services should contact the HMK Dental program officer.
Getting Assistance
Provider Relations field representatives can make onsite visits to train office staff on HMK/CHIP and Medicaid/HMK Plus billing procedures or to resolve claim payment issues.
Contact Provider Relations; the agent who takes the call will ask for a contact name, telephone number, and brief description of the issue, and forward the request to a Field Representative. The Field Representative will contact the provider and determine whether a field visit is necessary or whether the issue can be resolved by telephone or through a WebEx meeting.
Adjustment Request Form and Dental Claim Forms
American Dental Association (ADA) dental claim forms and the Current Dental Terminology (CDT) procedure code manual are not supplied by Conduent or DPHHS.
To order claim forms from the ADA, call 1-800-947-4746 or order online.
Department Responsibilities
The Montana Department of Public Health and Human Services (the Department) administers HMK/CHIP in Montana. HMK/CHIP was created by Congress to serve children from families with limited financial resource who do not qualify for Medicaid and who do not have medical health insurance.
Montana has chosen to purchase private insurance coverage for the majority of health services available to HMK/CHIP members. Dental services and eyeglasses are provided through private providers who contract with the Department. The Department is responsible for determining payment rates, benefit coverage, and member eligibility. The Department conducts oversight through retrospective utilization review.
This manual is a guide for the dental provider filing claims with HMK/CHIP. The manual is to be read and interpreted in conjunction with the General Information for Providers manual, federal regulations, state statutes, administrative procedures, and federally approved state plan amendments. This manual does not take precedence over federal regulation, state statutes, or administrative procedures.
For policy questions other than eligibility, call or write:
Healthy Montana Kids (HMK)/Children’s Health Insurance Program (CHIP)
Department of Public Health and Human Services
P.O. Box 202951
Helena, MT 59620-2951
(877) 543-7669 (Toll-free in Montana)
(888) 706-1535 (Montana Public Assistance)
Fiscal Agent Responsibilities
Conduent State Healthcare, LLC, is the fiscal agent for dental services for HMK/CHIP in Montana. Conduent processes claims and adjustments and responds to provider inquiries regarding claim status and payments.
End of General Information Chapter
Verifying HMK/CHIP Eligibility
How to Verify Eligibility
HMK/CHIP member eligibility must be verified at each provider visit. The child’s member ID number is on the HMK/CHIP Blue Cross and Blue Shield of Montana insurance card issued to each HMK/CHIP child.
Accurate recording of the 9-digit HMK/CHIP eligibility ID number is essential. Payment cannot be made for claims with incorrect HMK/CHIP ID numbers.
After obtaining the child’s HMK/CHIP ID number, verify member enrollment for the date of service by using one of the eligibility verification methods below.
- Provider Relations 1-800-624-3958 or 1-406-442-1837. Provider Relations is able to determine benefit limits; the methods below do not.
- FaxBack 1-800-714-0075 (24 hours). FaxBack will fax a report of the HMK/CHIP child’s eligibility. To sign up for FaxBack, call Provider Relations at 1-800-624-3958 (in/out of state) or 1-406-442-1837 (Helena). Your provider NPI and fax number are needed to sign up for this service, and your provider NPI and the child’s member ID number are needed to access this system.
- Integrated Voice Response (IVR) (800) 362-8312 (24 hours). Providers may verify whether a child is enrolled on a particular date of service. A touch-tone phone, your provider NPI, and the child’s member ID number are needed to access this system.
- Montana Access to Health (MATH) Web Portal . Contact Provider Relations to register or follow the instructions at https://mtaccesstohealth.portal.conduent.com/mt/general/home.do.
IVR, the MATH web portal, and FaxBack do not check program benefit limits. Information on benefit limits can only be obtained by contacting Provider Relations directly. Information on benefit limits is not a guarantee of payment. Information is available only for claims that have been processed. Claims that have been submitted, but not yet processed, may affect benefit limits.
The Department does not issue an eligibility card for HMK/CHIP dental benefits. The member will receive an insurance card with the HMK/CHIP member ID number. The insurance card is issued when a child is first enrolled in HMK/CHIP and is not recalled if HMK/CHIP enrollment ends, so the card cannot always be relied on to verify current eligibility.
Failure of Eligible HMK/CHIP Member to Notify Provider of HMK/CHIP Eligibility
An HMK/CHIP member must notify a provider that he/she has HMK/CHIP benefits. If the member fails to do this, he/she is responsible for the bill unless the provider agrees to discontinue billing the member and to submit a claim to HMK/CHIP.
If the provider agrees to bill HMK/CHIP, timely filing limits and coverage limits are applied.
HMK/CHIP Dental Benefit Plan
Effective July 1, 2014, the HMK/CHIP Dental Plan benefit is $1,900 for billable procedure codes that are paid at 85% for a total paid amount of $1615.
The benefit year for the HMK/CHIP dental benefit plan is July 1 through June 30 of the following year. The dentist will expect the member to pay for services that are over the limit of $1,900. All HMK/CHIP-enrolled children can obtain dental care under the Dental Plan.
End of Verifying HMK/CHIP Eligibility Chapter
Reimbursement, Covered, and Non-Covered Services
HMK/CHIP Reimbursement – Dental Plan
A child may receive up to $1,900 in dental services per benefit year from the Dental Plan. Dental services are reimbursed at 85% of the billed charges up to $1,615 ($1,900 x 85% = $1,615).
- Providers may not balance bill the child’s guardian for the remaining 15% of billed charges.
- Providers may bill the child's guardian for services in excess of $1,900.
- Dental services provided to an HMK/CHIP member must be billed to the address in the Key Contacts and Websites chapter.
- Only children age 5 and under are approved for hospital same-day surgery.
- Accident-related dental claims should be submitted to the HMK/CHIP office at the address listed in the Key Contacts section.
Payment from HMK/CHIP is payment in full for a covered service. Providers may never bill the HMK/CHIP member for:
- Billing errors that cause a claim to be denied, such as a wrong procedure code; an incorrectly completed claim form; or submission of a claim more than 365 days after the date of service.
- The balance between the $1,615 HMK/CHIP annual benefit and the first $1,900 in charges.
A provider can bill the HMK/CHIP member if:
- The member has been given a written explanation that a service is non-covered and he/she is responsible for the charges.
- The member is not HMK/CHIP-eligible at the time services are provided.
- The member has exceeded the HMK/CHIP Dental Plan benefit of $1,900 per benefit year.
Providers must comply with all applicable state and federal statutes, rules and regulations. These include the United States Codes governing HMK/CHIP and all applicable Montana statutes and rules governing licensure and certification.
Providers must also comply with the requirements governing HMK/CHIP to the extent that these provisions are not inconsistent with the HMK/CHIP rule requirements.
HMK/CHIP dental providers must first bill the child’s other dental insurance before they can submit dental claims to HMK/CHIP. The dental provider then submits the EOB from the primary dental insurance before HMK/CHIP reviews the claim. Fax the dental claim and EOB to 1-406-444-1861.
This is in accordance with 42 CFR 433.139, which establishes Medicaid and HMK/CHIP as the payer of last resort for all states.
Determining HMK/CHIP Reimbursement
HMK/CHIP pays 85% of billed charges up to $1,900 per member in a benefit year for the Dental Plan benefit. A benefit year is July 1 through June 30 of the following year.
Thus for the first $1,900 of charges, HMK/CHIP pays $1,615 ($1,900 x 85% = $1,615). This payment amount of $1,615 is payment in full for covered services that total $1,900.
An HMK/CHIP member may not be billed the difference (15%) between the HMK/CHIP payment amount and the provider’s charges, but the family can be billed for dental work over $1,900. Once an HMK/CHIP member is accepted as a patient, the provider may not agree to accept HMK/CHIP reimbursement for some services and not for others.
The $1,900 HMK/CHIP Dental Plan benefit is applicable to each enrolled child per benefit year (July 1–June 30). Your services and those services provided by other dentists are applied to this Dental Plan benefit.
An EOB code will appear on your Remittance Advice indicating the line item service billed was reduced or paid at zero because the $1,615 HMK/CHIP Dental benefit cap has been met. A portion of the line item charges may then be billable to the member.
Billing the Member
When the $1,900 Dental Plan benefit is exhausted, the HMK/CHIP member is responsible for payment for any additional services he/she wishes to have the provider perform.
HMK/CHIP will not enter into any dispute between the provider and the member regarding billing and payment issues. To avoid misunderstandings with HMK/CHIP members, providers are advised to obtain written confirmation from HMK/CHIP members whenever private payment arrangements are contemplated.
The HMK/CHIP member is also responsible for any services not covered by HMK/CHIP.
Covered Services
For a list of covered services, see https://medicaidprovider.mt.gov/18.
Non-Covered Services
HMK/CHIP does not cover orthodontic services (braces), maxiofacial surgeries and prosthetics, surgical procedures, and treatment of fractures.
HMK/CHIP does not cover experimental services and services generally regarded by dental professionals as unacceptable treatment, or any treatments that are not medically necessary.
Usual and Customary Charges
All charges for services submitted to HMK/CHIP must be made in accordance with an individual provider's usual and customary charges to the general public.
No-Show Appointments
Canceled or missed appointments by HMK/CHIP members cannot be billed to HMK/CHIP. If your office policy is to bill all patients for canceled or missed appointments, HMK/CHIP members may be billed for any no-show appointments.
Medical Necessity
All claims are subject to post-payment review for medical necessity by HMK/CHIP. Clinical records should substantiate the need for service by including the findings and information to support medical necessity and detailing the care rendered. If upon post-payment review the Department determines that services are not medically necessary, payment will be denied and action will be taken to recoup payment for those services. If the Department determines that a service was not medically necessary, the provider may not bill the HMK/CHIP member.
Each HMK/CHIP member’s clinical record must include sufficient documentation to enable the Department to determine the appropriateness of the treatment performed without requiring a member examination. Each page of documentation must have the signature of the treating dentist.
Each HMK/CHIP clinical record shall include, at a minimum, documentation of clinical diagnoses, pertinent medical and dental history, a treatment plan, complete anesthesia record if applicable, and any radiographs used to facilitate the development of the treatment plan. HMK/CHIP clinical records shall be maintained for 6 years and 3 months.
End of Reimbursement, Covered, and Non-Covered Services Chapter
Billing Procedure
Important Billing Guidelines
- Enter your NPI provider number as indicated on the 2012 ADA Claim Form.
- Enter your Provider Specialty code or Taxonomy code on line 56A of the 2012 ADA Claim Form.
- The Department prefers electronic media claim transmission.
- Effective January 1, 2015, the 2012 ADA Dental Claim Form is mandatory. CDT codes must be used.
- Use one claim per HMK/CHIP member.
- Claims must be submitted within 365 days of service.
- Date of submission is the date the claim is stamped as received by Conduent. If a claim is lost in the mail, the claim is not considered received.
- Information on the form must be legible.
- A clean or problem-free claim is usually processed within 35 days of receipt.
- Providers must register for electronic funds transfer (EFT).
- Payments for approved claims are deposited electronically into the account specified.
Coding Requirements – Current Dental Terminology, Dental Procedure Codes
Montana HMK/CHIP Coding Guidelines
CDT codes and their respective definitions were developed by the American Dental Association. These codes are used by HMK/CHIP for claim adjudication. HMK/CHIP has established specific guidelines for covered services and reimbursement. (See the Reimbursement, Covered, and Non-Covered Services chapter for details.)
Electronic Data Interchange (EDI) Transmissions
Conduent accepts electronic media, including direct entry (via telephone modem with PC) and File Transfer Protocol (FTP).
Submitting claims via electronic media speeds claims processing and increases accuracy. Providers may submit claims through an electronic medium or choose from a firm that offers electronic claim submission services for a per-claim fee. A provider contracts with a vendor to submit claims via one of the above methods.
WINASAP 5010
WINASAP 5010 is a Windows-based electronic claims entry application fo Montana Medicaid. This free software was developed as an alternative to submitting claims on paper. Providers may use it to submit claims for Montana Medicaid, MHSP, and HMK/CHIP (dental and eyeglasses only). It does not support submissions to Medicare or other payers. This software creates an 837 transaction, but does not accept an 835 (electronic remittance advice) transaction back from the Department. The software can be downloaded directly from the Provider Information website. For more information on WINASAP 5010, call the EDI Support Unit, 1 (800) 987-6719.
Providers are responsible for securing their own computer equipment, associated operating supplies, and modem to transmit via telephone lines.
Montana Users Guide for WINASAP 5010
The Montana Users Guide contains important information required for billing. Answers to most questions can be found by referencing the Montana Users Guide, including those regarding hardware requirements. Please read the Montana Users Guide prior to calling the EDI Support Unit with questions. Technical support is limited for this free software.
Paper Submission of Claims – ADA Dental Claim Form
Effective January 1, 2015, the 2012 ADA Dental Claim form is the only form on which to submit paper claims. Conduent and the Department do not supply the ADA Dental Claim Form. The ADA Dental Claim Form may be ordered from an independent printer or ADA Catalog Sales and Service at 1 (800) 947-4746.
Provider Specialty Codes
56A Provider Specialty Code
Enter the code that indicates the type of dental professional who delivered the treatment. Available codes describing treating dentists are listed below. The general code listed as “Dentist” may be used instead of any other dental practitioner code. The provider specialty code must be the same code as the dentist enrolled with at Conduent.
Code: 122300000X
Description: Dentist - A dentist is a person qualified by a doctorate in dental surgery (D.D.S.) or dental medicine (D.M.D.) licensed by the state to practice dentistry, and practicing within the scope of the license.
Code: 1223G0001X
Description: General Practice
Code: Various
Description: Dental Specialty
Code: 1223D0001X
Description: Dental Public Health
Code: 1223E0200X
Description: Endodontics
Code: 1223X0400X
Description: Orthodontics
Code: 1223P0221X
Description: Pediatric Dentistry
Code: 1223P0300X
Description: Periodontics
Code: 1223P0700X
Description: Prosthodontics
Code: 1223P0106X
Description: Oral and Maxillofacial Pathology
Code: 1223D0008X
Description: Oral and Maxillofacial Radiology
Code: 1223S0112X
Description: Oral and Maxillofacial Surgery
Authorized Signatures
All claims must be signed by the provider in Box 53 of the 2012 ADA form. The signature may be handwritten, a stamped facsimile, typed, or computer-generated, or be the signature of an authorized representative. The signature certifies that all information on the claim is believed to be true, accurate, and complete.
Where to Send Claims
Send completed ADA Dental Claim forms to:
Conduent Claims Processing
P.O. Box 8000
Helena, MT 59604
Timely Filing
Providers must submit a clean claim within 365 days of the date of service. A clean claim is one that can be processed for payment without correction or additional information or documentation from the provider. Timely filing cannot be waived when a claim is denied due to provider billing errors.
Follow-Up on Claim Resolution
Timely follow-up of claims is the provider’s responsibility. Events beyond a provider’s control may affect claims. Regardless of the cause of the problem, it is the provider’s responsibility to initiate appropriate action and follow-up to get claims issues resolved within the 365 day filing limit. The Department and Conduent Claims Processing will not know if a claim is lost in the mail or if a keying error is made. A provider is the only one who can identify when these problems occur and when assistance is necessary to resolve them.
It is important for providers to review paid and denied claims on each remittance advice and take corrective action to resolve denied claims. Correction of the problems listed on the remittance advice does not guarantee all problems have been resolved. The system will report all problems identified at the time the claim is processed. Additional errors may occur at the time of resubmission. Provider Relations is available to assist a provider who is having difficulty correcting and resubmitting a claim.
How to Appeal Timely Filing Denials
The provider’s appeal should be filed with HMK/CHIP, Department of Public Health and Human Services, P.O. Box 202951, Helena, MT 59620-2951, and should include the following:
- Documentation of previous claim submission
- An explanation of the problem
- A clean copy of the claim, along with any required documentation
Billing Tips to Avoid Timely Filing Denials
- File claims as soon as possible after services are provided.
- Carefully review error denial codes on the remittance advice including detail denial lines and additional errors reported beneath each claim.
- Resubmit the entire claim or denied detail line after all corrections have been made.
- If you have any questions regarding billing or denials, contact Provider Relations before resubmitting a claim.
- If you have not received payment within 45 days of submission, contact Provider Relations regarding the status of the claim.
- If you have had multiple denials on a claim, contact Provider Relations and request a review of the denials before resubmission.
Note: Once a provider has agreed to accept an HMK/CHIP member, any loss of HMK/CHIP reimbursement due to provider failure to meet timely filing deadlines is the responsibility of the provider. The provider may not bill the family for any service within the $1,900 cap.
The Remittance Advice
The remittance advice summarizes the status of claims submitted to HMK/CHIP for payment whether they were paid, suspended, or denied. Aside from providing a record of transactions, the remittance advice assists in resolving possible errors.
- Claims are grouped by disposition category. For example, paid, denied, and suspended claims, and claim adjustments are listed in separate sections.
- Claim Status – PAID group contains all the paid claims. If a claim has been paid that should not have been billed to HMK/CHIP, refer to How to File a Void or Adjustment Request in this chapter for instructions. Only a paid claim can be voided or adjusted.
- Claim Status – DENIED group reports denied claims. A denied claim can be resubmitted with new or additional information. (See the section titled How to Resubmit a Denied Claim in this chapter.)
- Claim Status – SUSPENDED group reports claims suspended for review. Do not rebill these claims. Suspended claims cannot be adjusted or voided. All claims in suspended status are reported each payment cycle until paid or denied.
- All paid, denied, and suspended claims and claim adjustments are itemized within each group in alphabetical order by member last name.
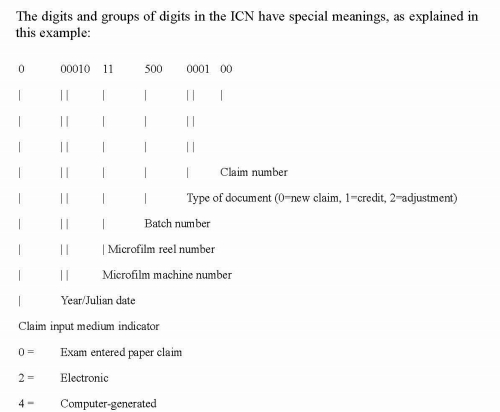
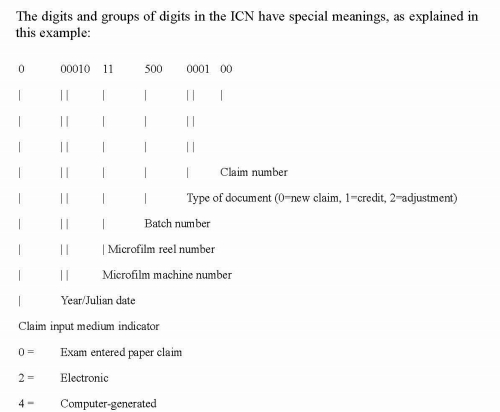
- Internal Control Numbers (ICNs) are assigned to all of the claims in the batch as they are microfilmed. The ICN assigned to each claim allows the claim to be tracked throughout the Montana HMK/CHIP system.
The remittance advice summary section reports the number of claim transactions, and total payment, or check amount. Each claim processed during the weekly cycle is listed on the remittance advice.
How to Resubmit a Denied Claim
Check the remittance advice before submitting a second request for payment. Claims should be resubmitted if the claim has not appeared on an remittance advice as paid, denied, or suspended and it has been 30 days since the claim was submitted; or the claim was denied due to incorrect or missing information.
Resubmit the claim on a new claim form or a legible photocopy after correcting any error or attaching requested documentation. Claims and attachments that cannot be clearly microfilmed or photocopied will be returned.
Adjustments
If a provider feels that a claim has been paid incorrectly and wants the claim to be adjusted, the provider must submit an Individual Adjustment Request form to Conduent.
An adjustment is a post-payment request by a provider to adjust a specific claim. No adjustment request can be submitted until a claim has been paid. Denied claims cannot be adjusted.
A provider should complete the adjustment request, attach a copy of the related remittance advice, and submit the form to Conduent, who reviews the adjustment requests for completeness and timely filing.
Adjustment requests must be submitted in accordance with the timely filing requirements. Incomplete forms or forms that are not received within the filing limit will be returned to the provider. Adjustment requests that pass the initial screening are submitted for processing.
When to Request an Adjustment
- Request an adjustment when a claim was overpaid or underpaid.
- Request an adjustment when a claim was paid but the information on the claim was incorrect (e.g., member ID, NPI, date of service, procedure code, diagnoses, units).
How to Request an Adjustment
To request an adjustment, use the Individual Adjustment Request form on the Forms page of the Provider Information website. The requirements for adjusting a claim are as follows:
- Claims must receive individual claim adjustment requests within 12 months from the date of service. After this time, gross adjustments are required.
- Use a separate Individual Adjustment Request form for each ICN. See the Forms page.
- If you are correcting more than one error per ICN, use only one Individual Adjustment Request form, and include each error on the form.
- If more than one line of the claim needs to be adjusted, indicate which lines and items need to be adjusted in the Remarks section of the adjustment form.
How to Complete an Adjustment Request
Adjustment requests must be submitted on the Individual Adjustment Request form. All pertinent information must be provided. Download the Individual Adjustment Request form from the website.
Complete Section A first with provider and member information and the claim’s ICN number. Complete Section B with information about the claim. Remember to fill in only the items that need to be corrected.
- Enter the date of service or the line number in the Date of Service or Line Number column.
- Enter the information from the claim form that was incorrect in the Information on Statement column.
- Enter the correct information in the column labeled Corrected Information.
How to Complete an Adjustment Request
Section A
Field: 1. Provider name and address
Description: Provider’s name and address (and mailing address if different).
Field: 2. Member name
Description: The member’s name.
Field: 3. Internal control number (ICN)
Description: There can be only one ICN per adjustment request form. When adjusting a claim that has been previously adjusted, use the ICN of the latest claim.
Field: 4. NPI
Description: The provider’s NPI.
Field: 5. Member HMK/CHIP number
Description: Member’s HMK/CHIP number.
Field: 6. Date of payment
Description: Date claim was paid is found on remittance advice.
Field: 7. Amount of payment
Description: The amount of payment from the remittance advice.
Section B
Field: 1. Units of service
Description: If a payment error was caused by an incorrect number of units, complete this line.
Field: 2. Procedure code/ NDC/Revenue code
Description: If the procedure code, NDC, or revenue code is incorrect, complete this line.
Field: 3. Dates of service (DOS)
Description: If the date of service is incorrect, complete this line.
Field: 4. Billed amount
Description: If the billed amount is incorrect, complete this line.
Field: 5. Personal resource (Nursing facility)
Description: If the member’s personal resource amount is incorrect, complete this line.
Field: 6. Insurance credit amount
Description: If the member’s insurance credit amount is incorrect, complete this line.
Field: 7. Net (Billed - TPL or Medicare paid)
Description: If the payment error was caused by a missing or incorrect insurance credit, complete this line. Net is billed amount minus the amount third party liability or Medicare paid.
Field: 8. Other/Remarks
Description: If none of the above items apply, or if you are unsure what caused the payment error, complete this line.
Adjustment requests will not be accepted by telephone. Correct all errors on the original claim form with one adjustment request by attaching a copy of the claim or remittance advice. Adjustments and voids are processed as replacement claims. In processing, the original payment is completely deducted and the adjustment is processed as a regular claim. The net result is a transaction that will increase or decrease your check.
Common Billing Errors
Reasons for Return or Denial: Provider NPI number and/or taxonomy number missing or invalid
How to Prevent Returned or Denied Claims: The NPI number is a 10-digit number assigned to the provider. Verify the correct NPI number and taxonomy are on the claim. The taxonomy is a 7-digit alphanumeric number indicating the provider’s specialty.
Reasons for Return or Denial: Authorized signature missing
How to Prevent Returned or Denied Claims: Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, handwritten, or computer-generated.
Reasons for Return or Denial: Signature date missing
How to Prevent Returned or Denied Claims: Each claim must have a signature date.
Reasons for Return or Denial: Incorrect claim form used
How to Prevent Returned or Denied Claims: The claim must be the correct form for the provider type. Services covered in this manual require a 2012 ADA claim form.
Reasons for Return or Denial: Information on claim form not legible
How to Prevent Returned or Denied Claims: Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Reasons for Return or Denial: Member number not on file, or member was not eligible on date of service
How to Prevent Returned or Denied Claims: Before providing services to the member, verify member eligibility by using one of the methods described in the Member Eligibility and Responsibilities chapter of the General Information for Providers manual. Eligibility may change monthly.
Reasons for Return or Denial: Prior authorization number is missing (implants only)
How to Prevent Returned or Denied Claims: Prior authorization is required for certain services, and the prior authorization number must be on the claim form.
Reasons for Return or Denial: Prior authorization does not match current information
How to Prevent Returned or Denied Claims: Claims must be billed and services performed during the prior authorization span. The claim will be denied if it is not billed according to the spans on the authorization.
Reasons for Return or Denial: Duplicate claim
How to Prevent Returned or Denied Claims: Check all remittance advices for previously submitted claims before resubmitting. When making changes to previously paid claims, submit an adjustment form rather than a new claim form.
Reasons for Return or Denial: TPL on file and no credit amount on claim
How to Prevent Returned or Denied Claims: If the member has any other insurance, bill the other carrier before HMK/CHIP.
If the member’s TPL coverage has changed, providers must notify the TPL Unit at the address in the Key Contacts pane on the Contact Us page of the Provider Information website before submitting a claim.
Reasons for Return or Denial: Claim past 365-day filing limit
How to Prevent Returned or Denied Claims: Conduent Claims Processing must receive all clean claims and adjustments within the timely filing limits described in this chapter.
To ensure timely processing, claims and adjustments must be mailed to Conduent Claims Processing at the address shown in Key Contacts .
Reasons for Return or Denial: Provider is not eligible during dates of services, enrollment has lapsed due to licensing requirements, or NPI terminated
How to Prevent Returned or Denied Claims: Out-of-state providers must update licensure for HMK/CHIP enrollment early to avoid denials. If enrollment has lapsed due to expired licensure, claims submitted with a date of service after the expiration date will be denied until the provider updates his/her enrollment.
New providers cannot bill for services provided before HMK/CHIP enrollment begins. If a provider is terminated from the HMK/CHIP program, claims submitted with a date of service after the termination date will be denied.
Reasons for Return or Denial: Procedure is not allowed for provider type
How to Prevent Returned or Denied Claims: Provider is not allowed to perform the service. Verify the procedure code is correct using current CDT Dental Procedure Codes. Verify the procedure code is valid for your provider type.
End of Billing Procedure Chapter
Provider Responsibilities
Provider Number
Providers who bill both Montana HMK/CHIP and Montana Medicaid have the same NPI number.
If a dental clinic is to be reimbursed for the dental work by a treating dentist, then the clinic must also have an NPI number.
Changes in Provider Enrollment
If any information you listed on your original provider enrollment application changes, you must notify Provider Enrollment in writing. Examples include but are not limited to change of address, change of tax identification number, cessation of practice, and lapse of license.
Send provider enrollment changes to:
Provider Enrollment
P.O. Box 4936
Helena, MT 59604
Recertification
Each year Conduent requests a copy of your license and other certification. This documentation must be submitted within 60 days of the request.
Provider Participation
A provider may choose to stop participating in HMK/CHIP at any time; however, a 30-day written notice of voluntary termination is requested. Notice should be addressed to Provider Relations.
Montana HMK/CHIP can terminate a provider's participation in HMK/CHIP for fraud, abuse, or other misuse of services. Reinstatement will be contingent upon provisions of State law.
Providers convicted of fraud or abuse in the Medicaid or Medicare programs may not participate in HMK/CHIP.
Accepting HMK/CHIP Members and Provider-Member Relationship
A dental provider can decide whether or not to become an HMK/CHIP provider and how many HMK/CHIP members to accept. This is true whether the member is new to the provider or is a current patient who becomes eligible for HMK/CHIP.
Providers must notify HMK/CHIP members prior to accepting them as a patient whether they will be accepted as an HMK/CHIP patient or as a private-pay patient.
If a provider fails to fulfill this responsibility, and an individual is an HMK/CHIP member, the state will assume that HMK/CHIP payment will be accepted.
If an HMK/CHIP member and the provider cannot agree on the financial terms of their relationship, either party can sever the relationship. As with any other patient, providers should ensure that services to a patient are not terminated in a manner that could be considered a violation of professional ethics considerations.
Record Keeping, Retention, and Access
The provider agreement requires that clinical records fully disclose the extent of services provided. Clinical record documentation should meet the following standards:
- The record must be legibly written.
- The record must identify the patient on each page.
- Entries must be signed and dated by the responsible licensed participating provider. Care rendered by personnel under the direct, personal supervision of the provider, in accordance with HMK/CHIP policy, must be countersigned by the responsible licensed, participating provider.
- The record must contain a preliminary working diagnosis and the elements of a history and physical examination upon which the diagnosis is based.
- All services and the treatment plan must be documented in the record. Any drugs prescribed as part of a treatment, including the quantities and the dosage, must be entered in the record.
- The record must indicate the observed medical condition of the patient, the progress at each visit, any change in diagnosis or treatment, and the patient’s response to treatment.
- Progress notes must be written for each visit billed to HMK/CHIP.
- Progress notes must be signed by the providing dentist.
Providers must retain clinical and financial records, including information regarding dates of service, diagnoses, services provided, and bills for services, for at least 6 years and 3 months from the end of the federal fiscal year (July 1–June 30) in which the services were rendered. If an audit is in progress, the records must be maintained until the audit is resolved.
HMK/CHIP providers must allow access to all records concerning services and payment to authorized personnel of the Montana Department of Public Health and Human Services, United States Department of Health and Human Services, State Auditor's Office, Montana Attorney General’s Office, and their designees. Records must be accessible to authorized personnel during normal business hours for the purpose of reviewing, copying, and reproducing documents. These entities shall have access to records even if the provider chooses to no longer participate in the program. Providers must furnish copies of claims and any other documentation upon request.
End of Provider Responsibilities Chapter
Appendix A: Forms
The forms listed below are available on the Forms page of the Provider Information website. The Dental Plan Fact Sheet is included in this chapter.
- Address Correction Form
- Individual Adjustment Form
- Paperwork Attachment Cover Sheet
- Dental Plan Fact Sheet
Dental Plan Fact Sheet
HMK/CHIP Dental Benefits
The Department of Public Health and Human Services (DPHHS) administers the Healthy Montana Kids (HMK)/CHIP program in Montana. DPHHS is responsible for determining payment rates, benefit coverage, member eligibility, and retrospective utilization review. A dentist enrolls as an HMK/CHIP provider through Conduent, LLC; the fiscal agent for the HMK/CHIP dental program. Conduent also processes dental claims and verifies benefits.
Billing and Payment Information
There are no copayments for HMK/CHIP covered dental services unless the child’s dental work goes over the $1,900 dental limit.
Effective July 1, 2014
- A child may receive up to $1,900 in reimbursable dental services per benefit year. Our benefit year now begins every July 1 through June 30 of the following year.
- Dental services are reimbursed at 85% of billed charges. HMK/CHIP dentists give a discount of 15% of the billed charges to the patent.
- At the 85% reimbursement rate, the maximum benefit to the dentist is $1,615. A code on the remittance advice indicates when the maximum has been paid.
- Only children age 5 or under are approved for same day hospital surgery and anesthesia for dental surgery. Bill Blue Cross and Blue Shield of Montana (BCBSMT) for the hospital and anesthesia services.
- Implant Services, CDT Codes D6000–D6199, are now covered with prior approval and proven medical necessity. The lifetime limit for implant services is $1,500 per person. Dental implants are included in the dental benefits.
- Dentists may charge families for services exceeding $1,900 per child per benefit year. Dentists and families can make payment arrangements.
- Dentists use the standard ADA billing forms and billing codes. Dental providers must use the 2012 ADA claim form effective January 2015.
A complete list of HMK covered dental codes can be found at hmk.mt.gov.
Contact Information
Submit dental claims to Conduent:
Conduent Claims Processing
P.O. Box 8000
Helena, MT 59604
Submit trauma-related dental claims to Healthy Montana Kids at the address at the bottom of the page. Claims will be processed under the medical benefit and submitted to the address below:
Healthy Montana Kids
P.O. Box 202951
Helena, MT 59620-2951
1-877-543-7669 (toll-free phone)
1-406-444-1861 (fax)
For claims information, MATH web portal information, or dental provider application, contact:
Conduent Provider Relations
P.O. Box 4936
Helena, MT 59604
1-800-624-3958 (In/Out of state)
406-442-1837 Helena
These telephone lines are open Monday through Friday, 8 a.m. to 5 p.m.
Verifying Eligibility for a Particular Date of Service
Below are several methods for verifying member eligibility.
Integrated Voice Response (IVR) (800) 362-8312
A touch-tone phone, your provider NPI, and the child’s member ID are needed to access this system.
Web Portal
The direct link to the MATH web portal is https://mtaccesstohealth.portal.conduent.com/mt/general/home.do. To access the web portal from the Montana Healthcare Programs Provider Information website, click the MATH Web Portal link in the gray box near the top of the page.
FaxBack 1-800-714-0075
FaxBack will fax a report of the HMK/CHIP child’s eligibility. To sign up for this service, call Montana Provider Relations at 1-800-624-3958 or 406-442-1837 in Helena. Your provider NPI and fax number are needed to sign up, and your provider NPI and the child’s member ID number are needed to access this system.
Additional Assistance
After contacting Montana Provider Relations, if you need additional assistance, contact the HMK/CHIP program officer at 1-877-543-7669 (toll-free) or at 406-444-7045 (Helena).
You may also contact HMK/CHIP by fax at 1-877-418-4533 or by mail at:
HMK/CHIP
P.O. Box 202951
Helena, MT 59620-2951
End of Appendix A: Forms Chapter
Definitions and Acronyms
End of Definitions and Acronyms Chapter
Index
Previous editions of this manual contained an index.
This edition has three search options.
1. Search the whole manual. Open the Complete Manual tab. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials"). The search box will show all locations where denials are discussed in the manual.
2. Search by chapter. Open any chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials"). The search box will show where denials are discussed in just that chapter.
3. Site search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs site specific search page.
End of Index Chapter
End of Healthy Montana Kids (HMK) and Children's Health Insurance Program (CHIP) Dental Services Manual
Update Log
Publication History
This publication supersedes all previous Physician-Related Services handbooks. Published by the Montana Department of Public Health & Human Services, January 2005.
Updated January 2003, October 2015, December 2015, August 2017, and August 2025
CPT codes, descriptions and other data only are copyright 2014 American Medical Association (or such other date of publication of CPT). All Rights reserved. Applicable FARS/DFARS Apply.
Update Log
08/22/2025
Deleted bulleted text in HMK/CHIP Reimbursement - Dental Plan section in the Reimbursement, covered, and Non-Covered Services chapter.
- Pre-approved medically necessary dental and orthodontic services only related to craniofacial anomaly or cleft palate are covered under the child's medical portion of HML/CHIP. This is handled through Children's Special Health Services.
08/03/2017
Healthy Montana Kids (HMK) and Children's Health Insurance Program (CHIP) Dental Services Manual converted to an HTML format and adapted to 508 Accessibility Standards. Additionally, updates were made throughout the manual.
12/31/2015
HMK and CHIP Dental, January 2016, HELP Plan-Related Updates and Others
10/05/2015
HMK and CHIP Dental, September 2015: Entire Manual
01/14/2003
HMK and CHIP Dental
Beginning in 2013, the format of the manual was changed. The manual was updated in July.
End of Update Log Chapter
Table of Contents
Key Contacts and Websites
General Information
Enrollment Information
Getting Assistance
Adjustment Request Form and Dental Claims Forms
Department Responsibilities
Fiscal Agent Responsibilities
Verifying HMK/CHIP Eligibility
How to Verify Eligibility
Failure of Eligible HMK/CHIP Member to Notify Provider of HMK/CHIP Eligibility
HMK/CHIP Dental Benefit Plan
Reimbursement, Covered, Non-Covered Services
HMK/CHIP Reimbursement - Dental Plan
Determining HMK/CHIP Reimbursement
Billing the Member
Covered Services
Non-Covered Services
Usual and Customary Charges
No-Show Appointments
Medical Necessity
Billing Procedures
Important Billing Guidelines
Coding Requirements - Current Dental Terminology, Dental Procedure Codes
Paper Submission of Claims - ADA Claim Form
Provider Specialty Codes
Authorized Signatures
Where to Send Claims
Timely Filing
Follow-Up on Claim Resolution
How to Appeal Timely Filing Denials
Billing Tips to Avoid Timely Filing Denials
The Remittance Advice
How to Resubmit a Dental Claim
Adjustments
Provider Responsibilities
Provider Number
Changes in Provider Enrollment
Recertification
Provider Participation
Accepting HMK/CHIP Members and Provider-Member Relationship
Record Keeping, Retention, and Access
Appendix A: Forms
Definitions and Acronyms
Index
End of Table of Contents Chapter
Key Contacts and Websites
Hours for Key Contacts are 8 a.m. to 5 p.m. Monday through Friday (Mountain Time), unless otherwise stated. For additional contacts and websites, see the Contact Us link in the left menu on the Montana Healthcare Programs Provider Information website.
Adjustment Requests
The Adjustment Request form and a sample dental form are on the Forms page of the Provider Information website.
American Dental Association (ADA) dental claim forms and the Current Dental Terminology (CDT) procedure code manual are not supplied by Conduent or DPHHS.
To order from the ADA, call 1-800-947-4746 or order online.
Dental Claims
Send dental claims to:
Conduent Claims Processing
P.O. Box 8000
Helena, MT 59604
1 (406) 442-2819 Fax
Dental Accident-Related Claims
Dental services related to an accident need to be reported to the HMK/CHIP Dental program officer for pre-approval. Dental accidents are covered through the child’s HMK/CHIP medical insurance plan. Providers of these services should contact the HMK/CHIP program officer for additional information.
Dental Program Officer
HMK/CHIP
P.O. Box 202951
Helena, MT 59620-2951
1 (406) 444-7045 Phone
1 (406) 444-1861 Fax
American Dental Association (ADA)
http://www.ada.org/en/
Information Available: The leading source of oral health related information for dentists and their patients.
Healthy Montana Kids (HMK)
https://dphhs.mt.gov/HMK
Information Available: Information on HMK/CHIP including eligibility, family and provider resources, enrollment, covered services, approved providers, copayments, how to become a provider, how to get a provider manual, and frequently asked questions.
InsureKidsNow.Gov
http://insurekidsnow.gov
Information Available: All states’ CHIP coverage and Find a Dentist feature.
End of Key Contacts and Websites Chapter
General Information
Enrollment Information
For information about becoming a Healthy Montana Kids (HMK) provider, contact Provider Relations or the HMK/CHIP Dental Unit.
Provider Relations
P.O. Box 4936
Helena, MT 59604
1 (800) 624-3958 In/Out of state
1 (406) 442-1837 Helena
HMK/CHIP Dental Unit
1 (877) 543-7669, X7045
1 (406) 444-7045
Dental services related to a trauma need to be reported to the HMK/CHIP Dental program officer for pre-approval. Dental trauma may be covered through the child’s HMK/CHIP medical benefit. Providers of these services should contact the HMK Dental program officer.
Getting Assistance
Provider Relations field representatives can make onsite visits to train office staff on HMK/CHIP and Medicaid/HMK Plus billing procedures or to resolve claim payment issues.
Contact Provider Relations; the agent who takes the call will ask for a contact name, telephone number, and brief description of the issue, and forward the request to a Field Representative. The Field Representative will contact the provider and determine whether a field visit is necessary or whether the issue can be resolved by telephone or through a WebEx meeting.
Adjustment Request Form and Dental Claim Forms
American Dental Association (ADA) dental claim forms and the Current Dental Terminology (CDT) procedure code manual are not supplied by Conduent or DPHHS.
To order claim forms from the ADA, call 1-800-947-4746 or order online.
Department Responsibilities
The Montana Department of Public Health and Human Services (the Department) administers HMK/CHIP in Montana. HMK/CHIP was created by Congress to serve children from families with limited financial resource who do not qualify for Medicaid and who do not have medical health insurance.
Montana has chosen to purchase private insurance coverage for the majority of health services available to HMK/CHIP members. Dental services and eyeglasses are provided through private providers who contract with the Department. The Department is responsible for determining payment rates, benefit coverage, and member eligibility. The Department conducts oversight through retrospective utilization review.
This manual is a guide for the dental provider filing claims with HMK/CHIP. The manual is to be read and interpreted in conjunction with the General Information for Providers manual, federal regulations, state statutes, administrative procedures, and federally approved state plan amendments. This manual does not take precedence over federal regulation, state statutes, or administrative procedures.
For policy questions other than eligibility, call or write:
Healthy Montana Kids (HMK)/Children’s Health Insurance Program (CHIP)
Department of Public Health and Human Services
P.O. Box 202951
Helena, MT 59620-2951
(877) 543-7669 (Toll-free in Montana)
(888) 706-1535 (Montana Public Assistance)
Fiscal Agent Responsibilities
Conduent State Healthcare, LLC, is the fiscal agent for dental services for HMK/CHIP in Montana. Conduent processes claims and adjustments and responds to provider inquiries regarding claim status and payments.
End of General Information Chapter
Verifying HMK/CHIP Eligibility
How to Verify Eligibility
HMK/CHIP member eligibility must be verified at each provider visit. The child’s member ID number is on the HMK/CHIP Blue Cross and Blue Shield of Montana insurance card issued to each HMK/CHIP child.
Accurate recording of the 9-digit HMK/CHIP eligibility ID number is essential. Payment cannot be made for claims with incorrect HMK/CHIP ID numbers.
After obtaining the child’s HMK/CHIP ID number, verify member enrollment for the date of service by using one of the eligibility verification methods below.
- Provider Relations 1-800-624-3958 or 1-406-442-1837. Provider Relations is able to determine benefit limits; the methods below do not.
- FaxBack 1-800-714-0075 (24 hours). FaxBack will fax a report of the HMK/CHIP child’s eligibility. To sign up for FaxBack, call Provider Relations at 1-800-624-3958 (in/out of state) or 1-406-442-1837 (Helena). Your provider NPI and fax number are needed to sign up for this service, and your provider NPI and the child’s member ID number are needed to access this system.
- Integrated Voice Response (IVR) (800) 362-8312 (24 hours). Providers may verify whether a child is enrolled on a particular date of service. A touch-tone phone, your provider NPI, and the child’s member ID number are needed to access this system.
- Montana Access to Health (MATH) Web Portal . Contact Provider Relations to register or follow the instructions at https://mtaccesstohealth.portal.conduent.com/mt/general/home.do.
IVR, the MATH web portal, and FaxBack do not check program benefit limits. Information on benefit limits can only be obtained by contacting Provider Relations directly. Information on benefit limits is not a guarantee of payment. Information is available only for claims that have been processed. Claims that have been submitted, but not yet processed, may affect benefit limits.
The Department does not issue an eligibility card for HMK/CHIP dental benefits. The member will receive an insurance card with the HMK/CHIP member ID number. The insurance card is issued when a child is first enrolled in HMK/CHIP and is not recalled if HMK/CHIP enrollment ends, so the card cannot always be relied on to verify current eligibility.
Failure of Eligible HMK/CHIP Member to Notify Provider of HMK/CHIP Eligibility
An HMK/CHIP member must notify a provider that he/she has HMK/CHIP benefits. If the member fails to do this, he/she is responsible for the bill unless the provider agrees to discontinue billing the member and to submit a claim to HMK/CHIP.
If the provider agrees to bill HMK/CHIP, timely filing limits and coverage limits are applied.
HMK/CHIP Dental Benefit Plan
Effective July 1, 2014, the HMK/CHIP Dental Plan benefit is $1,900 for billable procedure codes that are paid at 85% for a total paid amount of $1615.
The benefit year for the HMK/CHIP dental benefit plan is July 1 through June 30 of the following year. The dentist will expect the member to pay for services that are over the limit of $1,900. All HMK/CHIP-enrolled children can obtain dental care under the Dental Plan.
End of Verifying HMK/CHIP Eligibility Chapter
HMK/CHIP Reimbursement – Dental Plan
A child may receive up to $1,900 in dental services per benefit year from the Dental Plan. Dental services are reimbursed at 85% of the billed charges up to $1,615 ($1,900 x 85% = $1,615).
- Providers may not balance bill the child’s guardian for the remaining 15% of billed charges.
- Providers may bill the child's guardian for services in excess of $1,900.
- Dental services provided to an HMK/CHIP member must be billed to the address in the Key Contacts and Websites chapter.
- Only children age 5 and under are approved for hospital same-day surgery.
- Accident-related dental claims should be submitted to the HMK/CHIP office at the address listed in the Key Contacts section.
Payment from HMK/CHIP is payment in full for a covered service. Providers may never bill the HMK/CHIP member for:
- Billing errors that cause a claim to be denied, such as a wrong procedure code; an incorrectly completed claim form; or submission of a claim more than 365 days after the date of service.
- The balance between the $1,615 HMK/CHIP annual benefit and the first $1,900 in charges.
A provider can bill the HMK/CHIP member if:
- The member has been given a written explanation that a service is non-covered and he/she is responsible for the charges.
- The member is not HMK/CHIP-eligible at the time services are provided.
- The member has exceeded the HMK/CHIP Dental Plan benefit of $1,900 per benefit year.
Providers must comply with all applicable state and federal statutes, rules and regulations. These include the United States Codes governing HMK/CHIP and all applicable Montana statutes and rules governing licensure and certification.
Providers must also comply with the requirements governing HMK/CHIP to the extent that these provisions are not inconsistent with the HMK/CHIP rule requirements.
HMK/CHIP dental providers must first bill the child’s other dental insurance before they can submit dental claims to HMK/CHIP. The dental provider then submits the EOB from the primary dental insurance before HMK/CHIP reviews the claim. Fax the dental claim and EOB to 1-406-444-1861.
This is in accordance with 42 CFR 433.139, which establishes Medicaid and HMK/CHIP as the payer of last resort for all states.
Determining HMK/CHIP Reimbursement
HMK/CHIP pays 85% of billed charges up to $1,900 per member in a benefit year for the Dental Plan benefit. A benefit year is July 1 through June 30 of the following year.
Thus for the first $1,900 of charges, HMK/CHIP pays $1,615 ($1,900 x 85% = $1,615). This payment amount of $1,615 is payment in full for covered services that total $1,900.
An HMK/CHIP member may not be billed the difference (15%) between the HMK/CHIP payment amount and the provider’s charges, but the family can be billed for dental work over $1,900. Once an HMK/CHIP member is accepted as a patient, the provider may not agree to accept HMK/CHIP reimbursement for some services and not for others.
The $1,900 HMK/CHIP Dental Plan benefit is applicable to each enrolled child per benefit year (July 1–June 30). Your services and those services provided by other dentists are applied to this Dental Plan benefit.
An EOB code will appear on your Remittance Advice indicating the line item service billed was reduced or paid at zero because the $1,615 HMK/CHIP Dental benefit cap has been met. A portion of the line item charges may then be billable to the member.
Billing the Member
When the $1,900 Dental Plan benefit is exhausted, the HMK/CHIP member is responsible for payment for any additional services he/she wishes to have the provider perform.
HMK/CHIP will not enter into any dispute between the provider and the member regarding billing and payment issues. To avoid misunderstandings with HMK/CHIP members, providers are advised to obtain written confirmation from HMK/CHIP members whenever private payment arrangements are contemplated.
The HMK/CHIP member is also responsible for any services not covered by HMK/CHIP.
Covered Services
For a list of covered services, see https://medicaidprovider.mt.gov/18.
Non-Covered Services
HMK/CHIP does not cover orthodontic services (braces), maxiofacial surgeries and prosthetics, surgical procedures, and treatment of fractures.
HMK/CHIP does not cover experimental services and services generally regarded by dental professionals as unacceptable treatment, or any treatments that are not medically necessary.
Usual and Customary Charges
All charges for services submitted to HMK/CHIP must be made in accordance with an individual provider's usual and customary charges to the general public.
No-Show Appointments
Canceled or missed appointments by HMK/CHIP members cannot be billed to HMK/CHIP. If your office policy is to bill all patients for canceled or missed appointments, HMK/CHIP members may be billed for any no-show appointments.
Medical Necessity
All claims are subject to post-payment review for medical necessity by HMK/CHIP. Clinical records should substantiate the need for service by including the findings and information to support medical necessity and detailing the care rendered. If upon post-payment review the Department determines that services are not medically necessary, payment will be denied and action will be taken to recoup payment for those services. If the Department determines that a service was not medically necessary, the provider may not bill the HMK/CHIP member.
Each HMK/CHIP member’s clinical record must include sufficient documentation to enable the Department to determine the appropriateness of the treatment performed without requiring a member examination. Each page of documentation must have the signature of the treating dentist.
Each HMK/CHIP clinical record shall include, at a minimum, documentation of clinical diagnoses, pertinent medical and dental history, a treatment plan, complete anesthesia record if applicable, and any radiographs used to facilitate the development of the treatment plan. HMK/CHIP clinical records shall be maintained for 6 years and 3 months.
End of Reimbursement, Covered, and Non-Covered Services Chapter
Billing Procedure
Important Billing Guidelines
- Enter your NPI provider number as indicated on the 2012 ADA Claim Form.
- Enter your Provider Specialty code or Taxonomy code on line 56A of the 2012 ADA Claim Form.
- The Department prefers electronic media claim transmission.
- Effective January 1, 2015, the 2012 ADA Dental Claim Form is mandatory. CDT codes must be used.
- Use one claim per HMK/CHIP member.
- Claims must be submitted within 365 days of service.
- Date of submission is the date the claim is stamped as received by Conduent. If a claim is lost in the mail, the claim is not considered received.
- Information on the form must be legible.
- A clean or problem-free claim is usually processed within 35 days of receipt.
- Providers must register for electronic funds transfer (EFT).
- Payments for approved claims are deposited electronically into the account specified.
Coding Requirements – Current Dental Terminology, Dental Procedure Codes
Montana HMK/CHIP Coding Guidelines
CDT codes and their respective definitions were developed by the American Dental Association. These codes are used by HMK/CHIP for claim adjudication. HMK/CHIP has established specific guidelines for covered services and reimbursement. (See the Reimbursement, Covered, and Non-Covered Services chapter for details.)
Electronic Data Interchange (EDI) Transmissions
Conduent accepts electronic media, including direct entry (via telephone modem with PC) and File Transfer Protocol (FTP).
Submitting claims via electronic media speeds claims processing and increases accuracy. Providers may submit claims through an electronic medium or choose from a firm that offers electronic claim submission services for a per-claim fee. A provider contracts with a vendor to submit claims via one of the above methods.
WINASAP 5010
WINASAP 5010 is a Windows-based electronic claims entry application fo Montana Medicaid. This free software was developed as an alternative to submitting claims on paper. Providers may use it to submit claims for Montana Medicaid, MHSP, and HMK/CHIP (dental and eyeglasses only). It does not support submissions to Medicare or other payers. This software creates an 837 transaction, but does not accept an 835 (electronic remittance advice) transaction back from the Department. The software can be downloaded directly from the Provider Information website. For more information on WINASAP 5010, call the EDI Support Unit, 1 (800) 987-6719.
Providers are responsible for securing their own computer equipment, associated operating supplies, and modem to transmit via telephone lines.
Montana Users Guide for WINASAP 5010
The Montana Users Guide contains important information required for billing. Answers to most questions can be found by referencing the Montana Users Guide, including those regarding hardware requirements. Please read the Montana Users Guide prior to calling the EDI Support Unit with questions. Technical support is limited for this free software.
Paper Submission of Claims – ADA Dental Claim Form
Effective January 1, 2015, the 2012 ADA Dental Claim form is the only form on which to submit paper claims. Conduent and the Department do not supply the ADA Dental Claim Form. The ADA Dental Claim Form may be ordered from an independent printer or ADA Catalog Sales and Service at 1 (800) 947-4746.
Provider Specialty Codes
56A Provider Specialty Code
Enter the code that indicates the type of dental professional who delivered the treatment. Available codes describing treating dentists are listed below. The general code listed as “Dentist” may be used instead of any other dental practitioner code. The provider specialty code must be the same code as the dentist enrolled with at Conduent.
Code: 122300000X
Description: Dentist - A dentist is a person qualified by a doctorate in dental surgery (D.D.S.) or dental medicine (D.M.D.) licensed by the state to practice dentistry, and practicing within the scope of the license.
Code: 1223G0001X
Description: General Practice
Code: Various
Description: Dental Specialty
Code: 1223D0001X
Description: Dental Public Health
Code: 1223E0200X
Description: Endodontics
Code: 1223X0400X
Description: Orthodontics
Code: 1223P0221X
Description: Pediatric Dentistry
Code: 1223P0300X
Description: Periodontics
Code: 1223P0700X
Description: Prosthodontics
Code: 1223P0106X
Description: Oral and Maxillofacial Pathology
Code: 1223D0008X
Description: Oral and Maxillofacial Radiology
Code: 1223S0112X
Description: Oral and Maxillofacial Surgery
Authorized Signatures
All claims must be signed by the provider in Box 53 of the 2012 ADA form. The signature may be handwritten, a stamped facsimile, typed, or computer-generated, or be the signature of an authorized representative. The signature certifies that all information on the claim is believed to be true, accurate, and complete.
Where to Send Claims
Send completed ADA Dental Claim forms to:
Conduent Claims Processing
P.O. Box 8000
Helena, MT 59604
Timely Filing
Providers must submit a clean claim within 365 days of the date of service. A clean claim is one that can be processed for payment without correction or additional information or documentation from the provider. Timely filing cannot be waived when a claim is denied due to provider billing errors.
Follow-Up on Claim Resolution
Timely follow-up of claims is the provider’s responsibility. Events beyond a provider’s control may affect claims. Regardless of the cause of the problem, it is the provider’s responsibility to initiate appropriate action and follow-up to get claims issues resolved within the 365 day filing limit. The Department and Conduent Claims Processing will not know if a claim is lost in the mail or if a keying error is made. A provider is the only one who can identify when these problems occur and when assistance is necessary to resolve them.
It is important for providers to review paid and denied claims on each remittance advice and take corrective action to resolve denied claims. Correction of the problems listed on the remittance advice does not guarantee all problems have been resolved. The system will report all problems identified at the time the claim is processed. Additional errors may occur at the time of resubmission. Provider Relations is available to assist a provider who is having difficulty correcting and resubmitting a claim.
How to Appeal Timely Filing Denials
The provider’s appeal should be filed with HMK/CHIP, Department of Public Health and Human Services, P.O. Box 202951, Helena, MT 59620-2951, and should include the following:
- Documentation of previous claim submission
- An explanation of the problem
- A clean copy of the claim, along with any required documentation
Billing Tips to Avoid Timely Filing Denials
- File claims as soon as possible after services are provided.
- Carefully review error denial codes on the remittance advice including detail denial lines and additional errors reported beneath each claim.
- Resubmit the entire claim or denied detail line after all corrections have been made.
- If you have any questions regarding billing or denials, contact Provider Relations before resubmitting a claim.
- If you have not received payment within 45 days of submission, contact Provider Relations regarding the status of the claim.
- If you have had multiple denials on a claim, contact Provider Relations and request a review of the denials before resubmission.
Note: Once a provider has agreed to accept an HMK/CHIP member, any loss of HMK/CHIP reimbursement due to provider failure to meet timely filing deadlines is the responsibility of the provider. The provider may not bill the family for any service within the $1,900 cap.
The Remittance Advice
The remittance advice summarizes the status of claims submitted to HMK/CHIP for payment whether they were paid, suspended, or denied. Aside from providing a record of transactions, the remittance advice assists in resolving possible errors.
- Claims are grouped by disposition category. For example, paid, denied, and suspended claims, and claim adjustments are listed in separate sections.
- Claim Status – PAID group contains all the paid claims. If a claim has been paid that should not have been billed to HMK/CHIP, refer to How to File a Void or Adjustment Request in this chapter for instructions. Only a paid claim can be voided or adjusted.
- Claim Status – DENIED group reports denied claims. A denied claim can be resubmitted with new or additional information. (See the section titled How to Resubmit a Denied Claim in this chapter.)
- Claim Status – SUSPENDED group reports claims suspended for review. Do not rebill these claims. Suspended claims cannot be adjusted or voided. All claims in suspended status are reported each payment cycle until paid or denied.
- All paid, denied, and suspended claims and claim adjustments are itemized within each group in alphabetical order by member last name.
- Internal Control Numbers (ICNs) are assigned to all of the claims in the batch as they are microfilmed. The ICN assigned to each claim allows the claim to be tracked throughout the Montana HMK/CHIP system.
The remittance advice summary section reports the number of claim transactions, and total payment, or check amount. Each claim processed during the weekly cycle is listed on the remittance advice.
How to Resubmit a Denied Claim
Check the remittance advice before submitting a second request for payment. Claims should be resubmitted if the claim has not appeared on an remittance advice as paid, denied, or suspended and it has been 30 days since the claim was submitted; or the claim was denied due to incorrect or missing information.
Resubmit the claim on a new claim form or a legible photocopy after correcting any error or attaching requested documentation. Claims and attachments that cannot be clearly microfilmed or photocopied will be returned.
Adjustments
If a provider feels that a claim has been paid incorrectly and wants the claim to be adjusted, the provider must submit an Individual Adjustment Request form to Conduent.
An adjustment is a post-payment request by a provider to adjust a specific claim. No adjustment request can be submitted until a claim has been paid. Denied claims cannot be adjusted.
A provider should complete the adjustment request, attach a copy of the related remittance advice, and submit the form to Conduent, who reviews the adjustment requests for completeness and timely filing.
Adjustment requests must be submitted in accordance with the timely filing requirements. Incomplete forms or forms that are not received within the filing limit will be returned to the provider. Adjustment requests that pass the initial screening are submitted for processing.
When to Request an Adjustment
- Request an adjustment when a claim was overpaid or underpaid.
- Request an adjustment when a claim was paid but the information on the claim was incorrect (e.g., member ID, NPI, date of service, procedure code, diagnoses, units).
How to Request an Adjustment
To request an adjustment, use the Individual Adjustment Request form on the Forms page of the Provider Information website. The requirements for adjusting a claim are as follows:
- Claims must receive individual claim adjustment requests within 12 months from the date of service. After this time, gross adjustments are required.
- Use a separate Individual Adjustment Request form for each ICN. See the Forms page.
- If you are correcting more than one error per ICN, use only one Individual Adjustment Request form, and include each error on the form.
- If more than one line of the claim needs to be adjusted, indicate which lines and items need to be adjusted in the Remarks section of the adjustment form.
How to Complete an Adjustment Request
Adjustment requests must be submitted on the Individual Adjustment Request form. All pertinent information must be provided. Download the Individual Adjustment Request form from the website.
Complete Section A first with provider and member information and the claim’s ICN number. Complete Section B with information about the claim. Remember to fill in only the items that need to be corrected.
- Enter the date of service or the line number in the Date of Service or Line Number column.
- Enter the information from the claim form that was incorrect in the Information on Statement column.
- Enter the correct information in the column labeled Corrected Information.
How to Complete an Adjustment Request
Section A
Field: 1. Provider name and address
Description: Provider’s name and address (and mailing address if different).
Field: 2. Member name
Description: The member’s name.
Field: 3. Internal control number (ICN)
Description: There can be only one ICN per adjustment request form. When adjusting a claim that has been previously adjusted, use the ICN of the latest claim.
Field: 4. NPI
Description: The provider’s NPI.
Field: 5. Member HMK/CHIP number
Description: Member’s HMK/CHIP number.
Field: 6. Date of payment
Description: Date claim was paid is found on remittance advice.
Field: 7. Amount of payment
Description: The amount of payment from the remittance advice.
Section B
Field: 1. Units of service
Description: If a payment error was caused by an incorrect number of units, complete this line.
Field: 2. Procedure code/ NDC/Revenue code
Description: If the procedure code, NDC, or revenue code is incorrect, complete this line.
Field: 3. Dates of service (DOS)
Description: If the date of service is incorrect, complete this line.
Field: 4. Billed amount
Description: If the billed amount is incorrect, complete this line.
Field: 5. Personal resource (Nursing facility)
Description: If the member’s personal resource amount is incorrect, complete this line.
Field: 6. Insurance credit amount
Description: If the member’s insurance credit amount is incorrect, complete this line.
Field: 7. Net (Billed - TPL or Medicare paid)
Description: If the payment error was caused by a missing or incorrect insurance credit, complete this line. Net is billed amount minus the amount third party liability or Medicare paid.
Field: 8. Other/Remarks
Description: If none of the above items apply, or if you are unsure what caused the payment error, complete this line.
Adjustment requests will not be accepted by telephone. Correct all errors on the original claim form with one adjustment request by attaching a copy of the claim or remittance advice. Adjustments and voids are processed as replacement claims. In processing, the original payment is completely deducted and the adjustment is processed as a regular claim. The net result is a transaction that will increase or decrease your check.
Common Billing Errors
Reasons for Return or Denial: Provider NPI number and/or taxonomy number missing or invalid
How to Prevent Returned or Denied Claims: The NPI number is a 10-digit number assigned to the provider. Verify the correct NPI number and taxonomy are on the claim. The taxonomy is a 7-digit alphanumeric number indicating the provider’s specialty.
Reasons for Return or Denial: Authorized signature missing
How to Prevent Returned or Denied Claims: Each claim must have an authorized signature belonging to the provider, billing clerk, or office personnel. The signature may be typed, stamped, handwritten, or computer-generated.
Reasons for Return or Denial: Signature date missing
How to Prevent Returned or Denied Claims: Each claim must have a signature date.
Reasons for Return or Denial: Incorrect claim form used
How to Prevent Returned or Denied Claims: The claim must be the correct form for the provider type. Services covered in this manual require a 2012 ADA claim form.
Reasons for Return or Denial: Information on claim form not legible
How to Prevent Returned or Denied Claims: Information on the claim form must be legible. Use dark ink and center the information in the field. Information must not be obscured by lines.
Reasons for Return or Denial: Member number not on file, or member was not eligible on date of service
How to Prevent Returned or Denied Claims: Before providing services to the member, verify member eligibility by using one of the methods described in the Member Eligibility and Responsibilities chapter of the General Information for Providers manual. Eligibility may change monthly.
Reasons for Return or Denial: Prior authorization number is missing (implants only)
How to Prevent Returned or Denied Claims: Prior authorization is required for certain services, and the prior authorization number must be on the claim form.
Reasons for Return or Denial: Prior authorization does not match current information
How to Prevent Returned or Denied Claims: Claims must be billed and services performed during the prior authorization span. The claim will be denied if it is not billed according to the spans on the authorization.
Reasons for Return or Denial: Duplicate claim
How to Prevent Returned or Denied Claims: Check all remittance advices for previously submitted claims before resubmitting. When making changes to previously paid claims, submit an adjustment form rather than a new claim form.
Reasons for Return or Denial: TPL on file and no credit amount on claim
How to Prevent Returned or Denied Claims: If the member has any other insurance, bill the other carrier before HMK/CHIP.
If the member’s TPL coverage has changed, providers must notify the TPL Unit at the address in the Key Contacts pane on the Contact Us page of the Provider Information website before submitting a claim.
Reasons for Return or Denial: Claim past 365-day filing limit
How to Prevent Returned or Denied Claims: Conduent Claims Processing must receive all clean claims and adjustments within the timely filing limits described in this chapter.
To ensure timely processing, claims and adjustments must be mailed to Conduent Claims Processing at the address shown in Key Contacts .
Reasons for Return or Denial: Provider is not eligible during dates of services, enrollment has lapsed due to licensing requirements, or NPI terminated
How to Prevent Returned or Denied Claims: Out-of-state providers must update licensure for HMK/CHIP enrollment early to avoid denials. If enrollment has lapsed due to expired licensure, claims submitted with a date of service after the expiration date will be denied until the provider updates his/her enrollment.
New providers cannot bill for services provided before HMK/CHIP enrollment begins. If a provider is terminated from the HMK/CHIP program, claims submitted with a date of service after the termination date will be denied.
Reasons for Return or Denial: Procedure is not allowed for provider type
How to Prevent Returned or Denied Claims: Provider is not allowed to perform the service. Verify the procedure code is correct using current CDT Dental Procedure Codes. Verify the procedure code is valid for your provider type.
End of Billing Procedure Chapter
Provider Responsibilities
Provider Number
Providers who bill both Montana HMK/CHIP and Montana Medicaid have the same NPI number.
If a dental clinic is to be reimbursed for the dental work by a treating dentist, then the clinic must also have an NPI number.
Changes in Provider Enrollment
If any information you listed on your original provider enrollment application changes, you must notify Provider Enrollment in writing. Examples include but are not limited to change of address, change of tax identification number, cessation of practice, and lapse of license.
Send provider enrollment changes to:
Provider Enrollment
P.O. Box 4936
Helena, MT 59604
Recertification
Each year Conduent requests a copy of your license and other certification. This documentation must be submitted within 60 days of the request.
Provider Participation
A provider may choose to stop participating in HMK/CHIP at any time; however, a 30-day written notice of voluntary termination is requested. Notice should be addressed to Provider Relations.
Montana HMK/CHIP can terminate a provider's participation in HMK/CHIP for fraud, abuse, or other misuse of services. Reinstatement will be contingent upon provisions of State law.
Providers convicted of fraud or abuse in the Medicaid or Medicare programs may not participate in HMK/CHIP.
Accepting HMK/CHIP Members and Provider-Member Relationship
A dental provider can decide whether or not to become an HMK/CHIP provider and how many HMK/CHIP members to accept. This is true whether the member is new to the provider or is a current patient who becomes eligible for HMK/CHIP.
Providers must notify HMK/CHIP members prior to accepting them as a patient whether they will be accepted as an HMK/CHIP patient or as a private-pay patient.
If a provider fails to fulfill this responsibility, and an individual is an HMK/CHIP member, the state will assume that HMK/CHIP payment will be accepted.
If an HMK/CHIP member and the provider cannot agree on the financial terms of their relationship, either party can sever the relationship. As with any other patient, providers should ensure that services to a patient are not terminated in a manner that could be considered a violation of professional ethics considerations.
Record Keeping, Retention, and Access
The provider agreement requires that clinical records fully disclose the extent of services provided. Clinical record documentation should meet the following standards:
- The record must be legibly written.
- The record must identify the patient on each page.
- Entries must be signed and dated by the responsible licensed participating provider. Care rendered by personnel under the direct, personal supervision of the provider, in accordance with HMK/CHIP policy, must be countersigned by the responsible licensed, participating provider.
- The record must contain a preliminary working diagnosis and the elements of a history and physical examination upon which the diagnosis is based.
- All services and the treatment plan must be documented in the record. Any drugs prescribed as part of a treatment, including the quantities and the dosage, must be entered in the record.
- The record must indicate the observed medical condition of the patient, the progress at each visit, any change in diagnosis or treatment, and the patient’s response to treatment.
- Progress notes must be written for each visit billed to HMK/CHIP.
- Progress notes must be signed by the providing dentist.
Providers must retain clinical and financial records, including information regarding dates of service, diagnoses, services provided, and bills for services, for at least 6 years and 3 months from the end of the federal fiscal year (July 1–June 30) in which the services were rendered. If an audit is in progress, the records must be maintained until the audit is resolved.
HMK/CHIP providers must allow access to all records concerning services and payment to authorized personnel of the Montana Department of Public Health and Human Services, United States Department of Health and Human Services, State Auditor's Office, Montana Attorney General’s Office, and their designees. Records must be accessible to authorized personnel during normal business hours for the purpose of reviewing, copying, and reproducing documents. These entities shall have access to records even if the provider chooses to no longer participate in the program. Providers must furnish copies of claims and any other documentation upon request.
End of Provider Responsibilities Chapter
Appendix A: Forms
The forms listed below are available on the Forms page of the Provider Information website. The Dental Plan Fact Sheet is included in this chapter.
- Address Correction Form
- Individual Adjustment Form
- Paperwork Attachment Cover Sheet
- Dental Plan Fact Sheet
Dental Plan Fact Sheet
HMK/CHIP Dental Benefits
The Department of Public Health and Human Services (DPHHS) administers the Healthy Montana Kids (HMK)/CHIP program in Montana. DPHHS is responsible for determining payment rates, benefit coverage, member eligibility, and retrospective utilization review. A dentist enrolls as an HMK/CHIP provider through Conduent, LLC; the fiscal agent for the HMK/CHIP dental program. Conduent also processes dental claims and verifies benefits.
Billing and Payment Information
There are no copayments for HMK/CHIP covered dental services unless the child’s dental work goes over the $1,900 dental limit.
Effective July 1, 2014
- A child may receive up to $1,900 in reimbursable dental services per benefit year. Our benefit year now begins every July 1 through June 30 of the following year.
- Dental services are reimbursed at 85% of billed charges. HMK/CHIP dentists give a discount of 15% of the billed charges to the patent.
- At the 85% reimbursement rate, the maximum benefit to the dentist is $1,615. A code on the remittance advice indicates when the maximum has been paid.
- Only children age 5 or under are approved for same day hospital surgery and anesthesia for dental surgery. Bill Blue Cross and Blue Shield of Montana (BCBSMT) for the hospital and anesthesia services.
- Implant Services, CDT Codes D6000–D6199, are now covered with prior approval and proven medical necessity. The lifetime limit for implant services is $1,500 per person. Dental implants are included in the dental benefits.
- Dentists may charge families for services exceeding $1,900 per child per benefit year. Dentists and families can make payment arrangements.
- Dentists use the standard ADA billing forms and billing codes. Dental providers must use the 2012 ADA claim form effective January 2015.
A complete list of HMK covered dental codes can be found at hmk.mt.gov.
Contact Information
Submit dental claims to Conduent:
Conduent Claims Processing
P.O. Box 8000
Helena, MT 59604
Submit trauma-related dental claims to Healthy Montana Kids at the address at the bottom of the page. Claims will be processed under the medical benefit and submitted to the address below:
Healthy Montana Kids
P.O. Box 202951
Helena, MT 59620-2951
1-877-543-7669 (toll-free phone)
1-406-444-1861 (fax)
For claims information, MATH web portal information, or dental provider application, contact:
Conduent Provider Relations
P.O. Box 4936
Helena, MT 59604
1-800-624-3958 (In/Out of state)
406-442-1837 Helena
These telephone lines are open Monday through Friday, 8 a.m. to 5 p.m.
Verifying Eligibility for a Particular Date of Service
Below are several methods for verifying member eligibility.
Integrated Voice Response (IVR) (800) 362-8312
A touch-tone phone, your provider NPI, and the child’s member ID are needed to access this system.
Web Portal
The direct link to the MATH web portal is https://mtaccesstohealth.portal.conduent.com/mt/general/home.do. To access the web portal from the Montana Healthcare Programs Provider Information website, click the MATH Web Portal link in the gray box near the top of the page.
FaxBack 1-800-714-0075
FaxBack will fax a report of the HMK/CHIP child’s eligibility. To sign up for this service, call Montana Provider Relations at 1-800-624-3958 or 406-442-1837 in Helena. Your provider NPI and fax number are needed to sign up, and your provider NPI and the child’s member ID number are needed to access this system.
Additional Assistance
After contacting Montana Provider Relations, if you need additional assistance, contact the HMK/CHIP program officer at 1-877-543-7669 (toll-free) or at 406-444-7045 (Helena).
You may also contact HMK/CHIP by fax at 1-877-418-4533 or by mail at:
HMK/CHIP
P.O. Box 202951
Helena, MT 59620-2951
End of Appendix A: Forms Chapter
Definitions and Acronyms
End of Definitions and Acronyms Chapter
Index
Previous editions of this manual contained an index.
This edition has three search options.
1. Search the whole manual. Open the Complete Manual tab. From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials"). The search box will show all locations where denials are discussed in the manual.
2. Search by chapter. Open any chapter tab (for example the "Billing Procedures" tab). From your keyboard press the Ctrl and F keys at the same time. A search box will appear. Type in a descriptive or key word (for example "Denials"). The search box will show where denials are discussed in just that chapter.
3. Site search. Search the manual as well as other documents related to a particular search term on the Montana Healthcare Programs site specific search page.
End of Index Chapter
End of Healthy Montana Kids (HMK) and Children's Health Insurance Program (CHIP) Dental Services Manual